Infectious disease outbreaks are inevitable—but we can mitigate their effects by investing in prevention and preparedness
Benjamin Franklin once famously said, “An ounce of prevention is worth a pound of cure.” He also warned, “By failing to prepare, you are preparing to fail.” The importance of prevention has been all too evident in the catastrophic COVID-19 pandemic: so many lives lost, livelihoods disrupted, and economies shuttered. The pandemic has been painful, and it has been humbling, shattering expectations of which countries were best prepared for such a public health emergency. Despite their affluence and seemingly better preparation, many developed economies have experienced vastly higher death rates from COVID-19 than several developing economies, something few would have predicted before the virus spread around the globe.
We may not know how countries will perform in the next pandemic, but we can be certain that at some point, the world will once again face a dangerous infectious disease outbreak—perhaps sooner than we think. Even if the next pandemic is inevitable, we do not need to stumble into it blindly.
Loading component...
Metrics upended
In 2019, the Global Health Security Index ranked the United States as the country best prepared to manage an infectious disease outbreak and the United Kingdom as the next best prepared. Two years after the pandemic erupted, the United States has endured the highest global death toll from COVID-19, with more than 700,000 deaths, while the United Kingdom has recorded seven times more deaths than the 20,000 that its government chief scientific adviser suggested in March 2020 would be a “good outcome.” The Global Health Security rankings, based on more than one hundred questions about dozens of indicators and sub-indicators, were no match for the novel coronavirus.
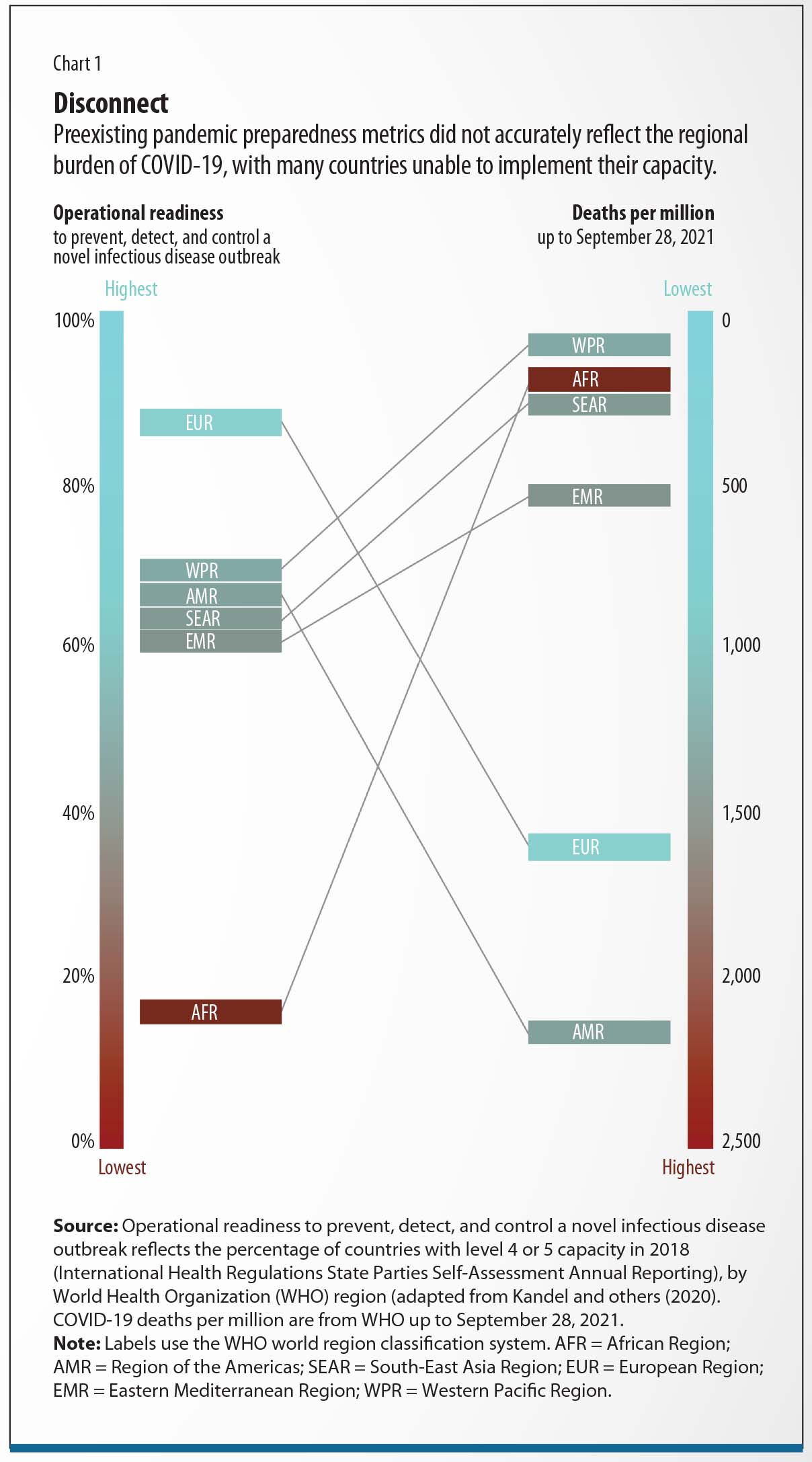
Similarly, based on a 2018 self-assessment of implementation of its International Health Regulations (IHR), the World Health Organization (WHO) deemed 86 percent of countries in Europe to be at the highest levels of pandemic preparedness, making the region the most prepared—at least on paper—to manage a novel infectious disease outbreak. In practice, Europe experienced the second highest death rate from COVID-19 of any region, at 1,294 per million people. Conversely in Africa, where the WHO considered just 15 percent of countries to be adequately prepared, fewer than 205 deaths per million have been reported (Chart 1).
Predictive metrics did not capture how experience with prior viral outbreaks would help West African countries combat COVID-19. In Liberia, reforms made in the wake of the 2014–16 Ebola outbreak to standardize and improve community-based health care proved beneficial when the first coronavirus cases were identified. In Sierra Leone, public health teams adapted targeted quarantine measures used for suspected and confirmed Ebola patients to isolate COVID-19 cases. Cross-country collaboration fostered in prior outbreaks also demonstrated value: in February 2020, Senegal’s Institut Pasteur de Dakar was one of only two laboratories in Africa able to test for SARS-CoV-2, with free tests yielding results within 24 hours or less. Staff at the Dakar lab shared their expertise and offered training to others outside Senegal, and by April 2020, 43 African countries had the capacity to effectively diagnose COVID-19.
Meanwhile, some of the world’s strongest health systems, including Italy’s Servizio Sanitario Nazionale, and some of the largest, including Brazil’s Sistema Único de Saúde, were shown to be woefully overstretched in the face of the pandemic, almost to the point of collapse. Even now, the provision of routine essential health care services remains fragile in these countries.
What went wrong in countries with seemingly resilient health infrastructures? As crystallized by American physician Paul Farmer, effective health care requires four key elements: “staff, stuff, space, and systems.” Amid the early escalation of community transmission, the UK government attempted to rapidly boost capacity by building seven emergency hospital facilities. It spent $736 million on these Nightingale Hospitals, which largely went unused even as existing hospital capacities neared a breaking point. The reason: adding space, stuff, and systems was futile without enough trained staff on hand.
In contrast, faced with early signs of local COVID-19 transmission, countries across sub-Saharan Africa and East Asia took a more bottom-up approach toward capacity building, thereby largely avoiding the need for lockdowns in 2020. Over four decades, Thailand had recruited a large network of volunteers, which was mobilized to assist in the logistical aspects of the response, providing coverage even in the most remote areas. In Vietnam, engaging existing local governance structures facilitated effective community-based coordination of quarantines and self-isolation. In Japan, rapidly training public health nurses allowed for thorough retrospective and prospective contact tracing, helping to identify the main clusters of transmission within the first few weeks of the outbreak. Implementing supportive interventions and conferring power on local government helped many countries curb transmission of the virus and avoid harsher, more sweeping measures.
Investing in prevention and preparedness
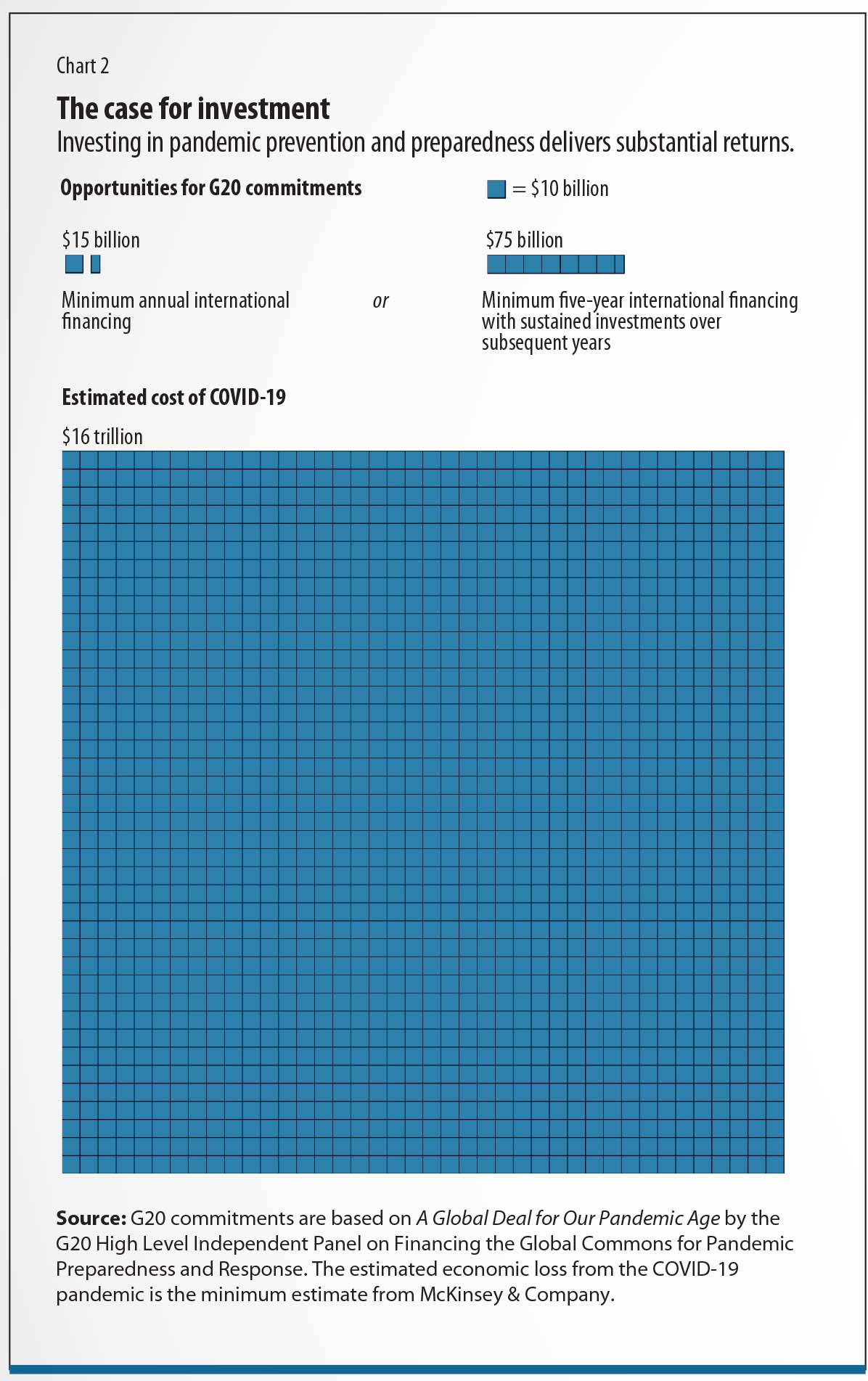
The COVID-19 pandemic has made the economic case for investing in health abundantly clear. Going forward, we must view health security as an investment rather than a cost; consider that by 2025, COVID-19 will have a global economic burden of $16–$35 trillion, according to estimates from McKinsey & Company and an independent G20 panel. If better preparedness reduced this cost even modestly, the return on investment, in absolute terms, would be substantial (Chart 2).
Policy differences aside, societies with a prevalence of chronic noncommunicable diseases and stark structural inequities fared poorly against the novel coronavirus. Rooting out both requires a long-term strategic plan but would be a key step toward securing a more sustainable world. Investing in health pays dividends twice over: first, in times of acute public health emergencies, including the growing challenge of antimicrobial resistance, and second, in building healthier and more equitable societies—both essential components of health security. Fortunately, for governments seeking short-term progress within election cycles, the latter delivers swift and continuous value in everyday health care. Finland’s government, for example, recognized that a good public health strategy for COVID-19 required agile and generous financing, but would offer payback from better fiscal protection and a speedier economic recovery.
Most health experts would not have described a pathogen triggering a pandemic as unprecedented but might use the term to describe the speed of scientific innovation and discovery throughout the COVID-19 pandemic. The development of multiple safe and effective COVID-19 vaccines was not the result of good luck but the fruit of decades of investment in scientific research. Governments built on their prior investments to accelerate the development and distribution of vaccines at a time when the world desperately needed therapeutic solutions. When addressing global health crises in the future, government support for science and technology, including amid periods of uncertainty, will be imperative.
The COVAX Facility, intended to ensure global vaccine equity, has underdelivered on its commitments. The mechanism to procure vaccines for low- to middle-income countries lacks the financial power to bring down prices, forcing COVAX to the back of the queue and reducing it to relying on donations. To echo a quote on the cover of a past issue of the Lancet: “rich countries behaved worse than anyone’s worst nightmares,” hoarding excess supplies of vaccines and, in the case of Canada, ordering doses equal to 10 times its population. Building and scaling up vaccine manufacturing hubs in low-income regions would help end the acute phase of the pandemic sooner and provide an infrastructure for combating other infectious diseases.
On a global level, the pandemic revealed deficiencies in health security agreements such as the IHR, which legally binds 196 countries to develop capacities to rapidly report and respond to disease outbreaks. As seen in the pandemic, many countries complied only in part, due to an incomplete awareness of the regulations or a deliberate flouting of them. Better compliance with the IHR surely would have resulted in responses that were timelier and more effective in safeguarding public health.
Loading component...
Although the pandemic exposed its shortcomings, the IHR remains indisputably central to the global health architecture for pandemics, and when adhered to, can be meaningful in any health emergency. Adjustments are needed, especially to adopt a more nuanced alerting mechanism and empower the WHO to continually review and improve member states’ compliance with the overall regime. For a revamped IHR to succeed, the WHO must have the financial support, authority, and trust needed to ensure better compliance with these potentially life-saving regulations. An increase in funding of $1 billion a year in assessed contributions for the WHO would be a start.
Successes and failures in the COVID-19 pandemic have shown us what we must do to be better prepared for the next pandemic. And, as Benjamin Franklin warned, if we fail to prepare for that event, we must be prepared to fail again—and to suffer the consequences.
This article draws on Devi Sridhar’s forthcoming book, Preventable: The Politics of Pandemics and How to Stop the Next One.
Opinions expressed in articles and other materials are those of the authors; they do not necessarily reflect IMF policy.
References:
Group of Twenty (G20). 2021. “A Global Deal for Our Pandemic Age.” Report of the High Level Independent Panel on Financing the Global Commons for Pandemic Preparedness and Response.
Kandel, N., S. Chungong, A. Omaar, and J. Xing. 2020. “Health Security Capacities in the Context of COVID-19 Outbreak: An Analysis of International Health Regulations Annual Report Data from 182 countries.” Lancet 395 (10229): 1047–53.
McKinsey & Company. 2021. “How Might the COVID-19 Pandemic End?” July 19.








